Introduction
Since the World Health Organization’s groundbreaking Commission on Social Determinants of Health (2008), the evidence has continued to grow about how factors beyond the medical drive poor health outcomes for individuals and communities.
These factors include poor-quality housing, unstable or insecure work and family breakdown. Meanwhile, in 2012 a landmark Australian study into legal need established that over one-fifth of people in Australia experience three or more legal problems in a given year, many of which cause illness. Many people seek no advice for these problems, but when they do, they are more likely to ask a non-legal advisor, such as a health professional, than a lawyer.
Taken together, the health and legal research points to common groups who are vulnerable to intersecting health and legal issues, but are more likely to turn to non-legal advisors, such as health professionals, than legal services for solutions.
Health justice partnerships respond to this evidence. In what has been a quiet revolution in service delivery, community lawyers have been collaborating with health services and their patients to address unmet, health-harming legal need. Since 2012 this revolution has grown from a handful of examples across the country to many. Now, through this report, we are able to identify the range of approaches, partnerships, settings and needs being met through health justice partnerships.
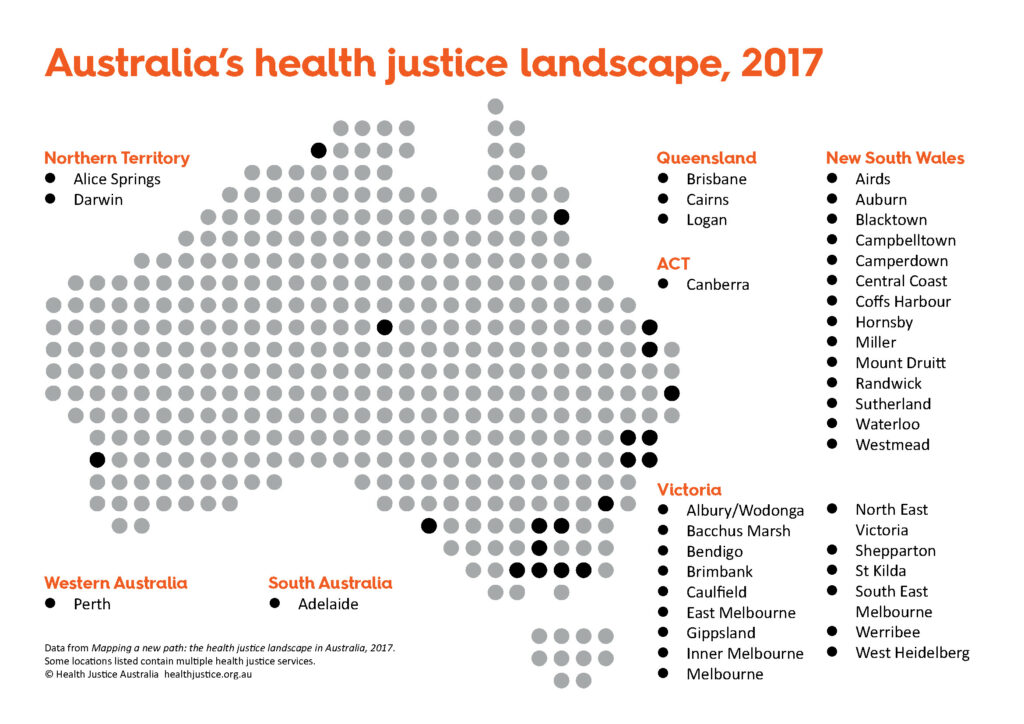
This report provides a first and foundational profile of the health justice landscape across Australia. It is based on information gathered in a 2017 survey, conducted by Health Justice Australia, of services across Australia that identify as health justice partnerships (hereafter, the services).
Growth on the landscape
The survey illustrates a health justice landscape that has grown from seven services in 2014 to include now:
- up to 30 services operating in partnership, integrating a lawyer into the healthcare team in a health setting
- a further 18 services delivering a range of other service models such as: integrated services (health and legal services provided by one organisation); service hubs (health and legal services joined with other services in a community setting); outreach (with less intensive partnership arrangements and more autonomy than health justice partnerships); and student clinics (partnerships between law faculties and health agencies).
The services have been operating in almost every state and territory in Australia, however most are in Victoria and New South Wales. Across Australia, three-quarters of all services are in major cities.
Where are services operating
Hospitals are the most common service setting, followed by community or public health service settings and Aboriginal medical or community services. While some partnerships assist any patient of the health service, most focus on a particular client group: women facing domestic or family violence, Aboriginal and Torres Strait Islander peoples, people with mental health issues, older people at risk of elder abuse or young people. Services most commonly provide legal help for domestic and family violence and for family and civil law issues. More than one in five respondents indicated that their partnership engaged in systemic advocacy.
Community legal centres were involved as legal partners in three-quarters of all partnerships and legal aid commissions in nearly three in ten. Public/not-for-profit hospitals and/or the area health services which administer them were partners in 28 services, community based health services in 14 services and Aboriginal community controlled health organisations in six.
A key feature of the landscape is the extent to which partners have supported each other with training and secondary consultation. More commonly, the help is provided by lawyers to their healthcare partners.
The shared goals of partnerships include: improving access to legal help, particularly to address health harming legal need; the provision of holistic services; improved client health and wellbeing; and improved legal outcomes for clients/patients.
Half of all services were mostly funded by government sources. However this first survey did not explore how secure this funding was and services have reported to Health Justice Australia that they face very real challenges in sustaining their health justice partnerships due to short-term and uncertain funding.
More mapping a new path content
A series of reports
This is one of three reports based on the mapping survey. The purpose of this first report is to provide a baseline picture of the health justice landscape, noting the range of services currently identifying as health justice partnerships. It provides foundational information to support planning, evaluation and the development of a best practice health justice partnership model, which is informed by the experience of practitioners and their partnerships.
The second, Service models on the health justice landscape: A closer look at partnership, is a discussion paper exploring what differentiates a health justice partnership from the other service models on the health justice landscape. This paper aims to develop clarity around the features of health justice partnerships as a specific service model. This understanding is critical to their effective evaluation.
A third report, Building health justice partnerships: 3 key lessons from practitioners, captures the experiences of health and legal practitioners in establishing partnerships between health and legal agencies to address health-harming legal need.



